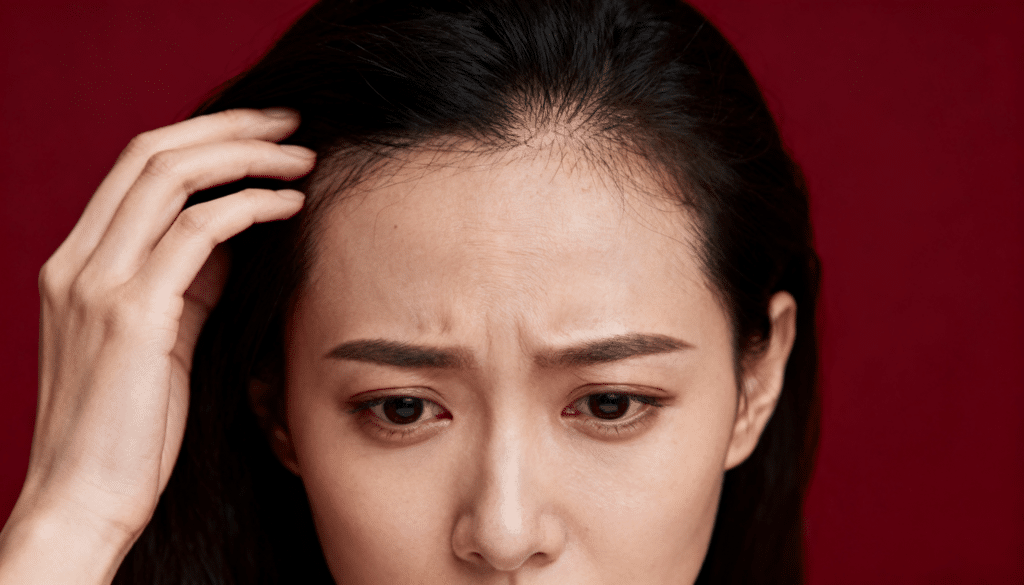
Many people with eczema notice their hair thinning or falling out more than usual, and they wonder if there’s a connection.
The constant itching, scratching, and inflammation that comes with eczema can indeed affect hair health in several ways. While eczema itself doesn’t directly cause hair loss, the behaviors and conditions it creates often do.
This blog will explain can eczema cause hair loss, from scalp inflammation to excessive scratching habits.
By understanding this connection, people can take steps to minimize hair damage and maintain healthier locks despite their eczema challenges.
The Different Types of Eczema
Scalp eczema is a form of dermatitis that affects the skin on the head, causing red, inflamed, and itchy patches.
It often appears as flaky, scaly areas that can be mistaken for dandruff, but the symptoms are typically more severe and persistent.
1. Atopic Dermatitis
This chronic condition typically begins in childhood and runs in families with allergies or asthma.
On the scalp, it creates intensely itchy, red patches that can become thick and leathery from constant scratching. The inflammation often spreads beyond the hairline to affect the face and neck areas, too.
2. Contact Dermatitis
This type develops when the scalp reacts to specific irritants like harsh shampoos, hair dyes, or styling products. Symptoms include redness, swelling, and burning sensations that appear shortly after exposure.
The reaction can range from mild irritation to severe blistering, depending on the trigger substance and individual sensitivity levels.
3. Seborrheic Dermatitis
Often mistaken for severe dandruff, this condition causes greasy, yellowish scales on the scalp along with redness and itching.
It’s linked to an overgrowth of yeast that naturally lives on the skin. The scales tend to be thicker and more stubborn than typical dandruff flakes, requiring specialized treatment approaches.
4. Dyshidrotic Eczema
Though more common on hands and feet, this type can occasionally affect the scalp area. It’s characterized by small, fluid-filled blisters that appear in clusters and cause intense itching.
The blisters eventually dry up and peel, leaving the skin raw and vulnerable to infection from scratching or external irritants.
5. Nummular Eczema
This distinctive form creates coin-shaped patches of irritated skin that can appear on the scalp. The round lesions are typically very itchy and may ooze or become crusty.
These patches can persist for months without proper treatment and often leave darker or lighter spots on the skin after healing completely.
6. Stasis Dermatitis
While primarily affecting the lower legs due to poor circulation, this type can sometimes occur on the scalp in people with certain medical conditions.
It causes swelling, redness, and scaling that worsens over time. The affected skin may develop a brownish discoloration and become increasingly thick and rough to the touch.
Note: The type of eczema most responsible for hair loss is seborrheic dermatitis, which causes scalp inflammation, itching, and follicle damage, leading to hair loss.
What Causes Seborrheic Dermatitis?

Seborrheic dermatitis stems from multiple factors working together, but the primary culprit is an overgrowth of Malassezia yeast that naturally lives on everyone’s skin.
This yeast feeds on the oils produced by sebaceous glands, and when it multiplies excessively, it triggers an inflammatory response that leads to the characteristic scaling and redness.
Several factors contribute to this yeast overgrowth. Hormonal changes, particularly increased androgen levels, can boost oil production and create an ideal environment for Malassezia.
Stress weakens the immune system’s ability to keep yeast levels in check, while certain medical conditions like Parkinson’s disease or HIV can increase susceptibility.
Cold, dry weather often worsens symptoms by disrupting the skin’s natural barrier.
Additionally, some people have a genetic predisposition that makes their immune system overreact to the yeast’s presence, creating chronic inflammation.
Can Eczema Cause Hair Loss?
Seborrheic dermatitis doesn’t directly destroy hair follicles, but it creates conditions that lead to temporary hair loss through several mechanisms.
The chronic inflammation weakens hair roots and disrupts the normal growth cycle, causing hairs to enter the resting phase prematurely.
Constant scratching is a major contributor to hair loss. The mechanical damage from fingernails breaks hair strands and can traumatize follicles, leading to increased shedding.
Additionally, the thick, greasy scales can clog hair follicles, restricting healthy growth and causing existing hairs to become loose and fall out more easily.
The inflammatory process also affects blood circulation to the scalp, reducing nutrient delivery to hair follicles. While this hair loss is typically temporary and reversible with proper treatment, untreated severe cases may result in prolonged thinning until the underlying inflammation is controlled.
Symptoms of Seborrheic Dermatitis Affecting the Scalp
Seborrheic dermatitis presents with several distinct symptoms that can significantly impact daily life.
These symptoms often fluctuate in severity, sometimes improving temporarily before flaring up again, making the condition particularly frustrating for those affected.
Greasy, Yellow Scales
The most characteristic symptom involves thick, oily flakes that adhere firmly to the scalp and hair strands. These scales have a distinctive yellowish color and greasy texture that sets them apart from regular dandruff.
They’re often difficult to remove with regular shampooing and tend to accumulate in patches, particularly around the hairline and crown area.
Red, Inflamed Patches
Areas of the scalp become visibly red and swollen, indicating active inflammation beneath the surface. These patches feel warm to the touch and may be tender or sensitive.
The redness often extends beyond the immediate affected area, creating irregular borders that can spread if the condition worsens or isn’t properly treated with appropriate medications.
Intense Itching
Persistent itching is one of the most bothersome symptoms, often becoming worse during stress or weather changes. The urge to scratch can be overwhelming, especially at night when distractions are minimal.
This constant itching disrupts sleep patterns and daily activities, creating a cycle where scratching provides temporary relief but ultimately worsens the underlying inflammation.
Flaking and Scaling
Unlike typical dandruff, these flakes are larger, thicker, and more stubborn to remove from the hair and scalp. The scales can be white or yellowish and often leave visible residue on clothing, particularly dark-colored shirts.
This symptom can be socially embarrassing and requires frequent hair washing, which sometimes irritates the condition further.
Hair Thinning
Chronic inflammation and excessive scratching can weaken hair follicles, leading to temporary hair loss in affected areas. While the hair typically regrows once inflammation subsides, persistent cases may result in more noticeable thinning.
The combination of scratching, harsh treatments, and inflammatory processes can damage the hair shaft and disrupt the normal growth cycle significantly.
Burning or Stinging Sensation
Many people experience a burning or stinging feeling, particularly when applying hair products or during flare-ups. This sensation can be intense enough to interfere with regular hair care routines.
The discomfort often worsens with heat, sweating, or when using products containing alcohol or strong fragrances that further irritate the already sensitive scalp tissue.
Crusty Patches
In severe cases, the scales can form thick, crusty patches that feel rough and raised above the normal scalp level. These areas may crack or bleed if disturbed, creating potential entry points for bacterial infections.
The crusty texture makes hair styling difficult and can trap odors, requiring specialized treatment approaches to soften and remove the buildup safely
Risk Factors and Triggers for Seborrheic Dermatitis

Several factors can increase the likelihood of developing seborrheic dermatitis or trigger flare-ups in those already affected.
Understanding these risk factors helps people identify potential triggers and take preventive measures to manage their condition more effectively.
1. Stress and Fatigue
High stress levels and chronic fatigue weaken the immune system’s ability to regulate yeast overgrowth on the scalp. Emotional stress triggers hormonal changes that increase oil production.
It creates ideal conditions for Malassezia yeast to flourish. Sleep deprivation further compromises immune function, making flare-ups more likely during challenging periods.
2. Hormonal Changes
Fluctuating hormone levels, particularly during puberty, pregnancy, or menopause, can trigger seborrheic dermatitis episodes. Increased androgen production stimulates sebaceous glands to produce more oil.
It feeds the yeast that causes inflammation. Men are more frequently affected due to naturally higher androgen levels throughout their lives.
3. Cold, Dry Weather
Winter conditions with low humidity and cold temperatures can worsen seborrheic dermatitis symptoms significantly. Dry air strips moisture from the scalp, disrupting the skin barrier and allowing irritants to penetrate more easily.
Indoor heating systems further reduce humidity levels, creating an environment that promotes flaking and inflammation.
4. Certain Medical Conditions
Neurological disorders like Parkinson’s disease, epilepsy, and spinal cord injuries increase susceptibility to seborrheic dermatitis. HIV infection and other immune-compromising conditions also elevate risk.
These medical conditions affect the body’s ability to regulate skin flora and maintain proper immune responses against yeast overgrowth.
5. Medications
Some medications can trigger or worsen seborrheic dermatitis symptoms as side effects. Lithium, used for bipolar disorder, commonly causes skin problems, including scalp inflammation.
Certain antipsychotic drugs and medications that suppress immune function can also increase vulnerability to yeast overgrowth and subsequent dermatitis development.
6. Genetic Predisposition
Family history plays a significant role in seborrheic dermatitis development, suggesting strong genetic components. People with relatives who have the condition are more likely to develop it themselves.
Genetic factors influence immune system responses to Malassezia yeast and determine individual sensitivity levels to inflammatory triggers.
7. Poor Hygiene Habits
Infrequent hair washing allows oil and dead skin cells to accumulate, providing nutrients for yeast growth. However, overwashing with harsh products can also trigger inflammation by stripping natural protective oils.
Finding the right balance in cleansing frequency and product selection is crucial for preventing flare-ups and maintaining scalp health.
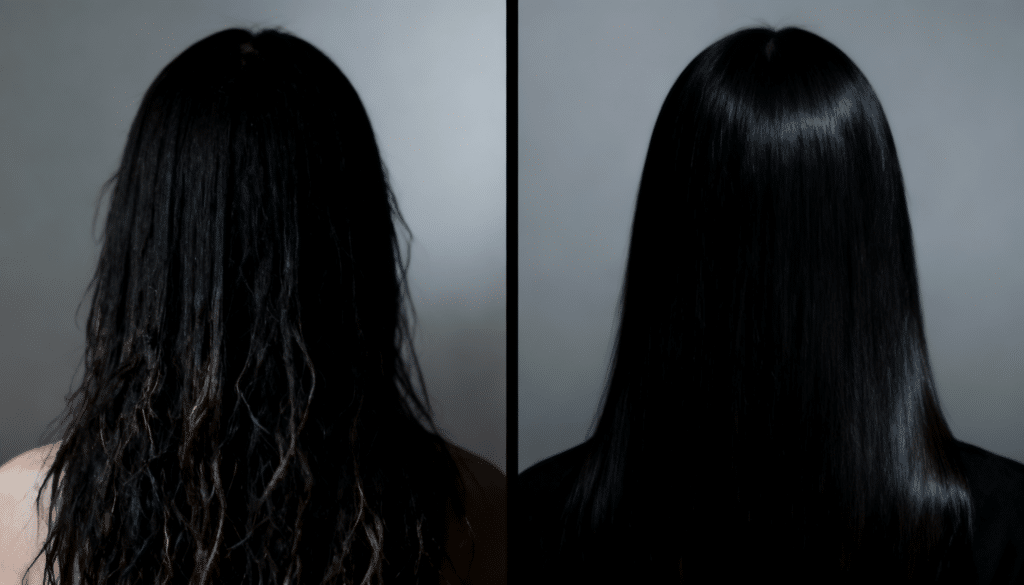
How Can Seborrheic Dermatitis Be Treated?
Seborrheic dermatitis treatment focuses on controlling yeast overgrowth, reducing inflammation, and managing symptoms.
Medicated shampoos containing antifungal ingredients like ketoconazole, selenium sulfide, or zinc pyrithione are first-line treatments that help control Malassezia yeast levels.
For severe cases, doctors may prescribe topical corticosteroids to reduce inflammation quickly, though these should be used sparingly to avoid side effects.
Antifungal creams or lotions can be applied directly to affected areas for targeted treatment. Maintaining consistent hair care routines with gentle, fragrance-free products helps prevent flare-ups.
Some people benefit from natural remedies like tea tree oil or apple cider vinegar, though these should be used cautiously. Regular stress management and adequate sleep also support treatment effectiveness.
When to Consult a Dermatologist Regarding Eczema?
See a dermatologist if scalp symptoms persist despite using over-the-counter treatments for several weeks. Severe itching that disrupts sleep or daily activities requires professional evaluation.
Signs of infection, like pus, increased redness, or warmth, need immediate attention. Consult a specialist when hair loss becomes noticeable or concerning.
If symptoms spread beyond the scalp to other body areas, professional treatment is necessary. People with underlying medical conditions should seek early intervention.
Don’t delay consultation if symptoms worsen rapidly or cause significant discomfort. Early treatment prevents complications and improves outcomes.
What Other Conditions Can Be Mistaken for Scalp Eczema?
Scalp eczema can look a lot like other skin problems, especially when symptoms overlap. Redness, flaking, itching, and even scabbing can be caused by many different conditions
| Condition | Main Symptoms | Key Differences from Scalp Eczema |
|---|---|---|
| Psoriasis | Thick, silvery scales; red patches; itching | Patches are often thicker and more sharply defined; they may extend beyond the scalp (like elbows or knees) |
| Seborrheic Dermatitis | Greasy scales, redness, dandruff | Very similar to scalp eczema; sometimes used interchangeably; triggered more by yeast overgrowth |
| Tinea Capitis (Ringworm) | Round bald patches, broken hairs, scaling | Caused by a fungal infection, often seen in children; requires antifungal treatment |
| Contact Dermatitis | Itchy rash, burning, redness after using products | Triggered by specific allergens or irritants (like shampoo); stops when product use is discontinued |
| Lichen Planopilaris | Hair loss, redness, scaling, pain, or burning | Involves permanent hair loss and scarring, more serious than scalp eczema |
| Folliculitis | Small red or white pus-filled bumps around hair follicles | More of a bacterial infection; feels sore or tender; not typically flaky like eczema |
The Bottom Line
Managing hair loss due to eczema requires understanding the connection between scalp inflammation and hair health.
Seborrheic dermatitis, the most common form affecting the scalp, creates a cycle where yeast overgrowth leads to inflammation, scratching, and eventual hair thinning.
Remember, professional guidance from a dermatologist can accelerate recovery and prevent complications.
Taking action early protects both scalp health and hair density long-term.